Symptothermal Method: Empowering Reproductive Choices

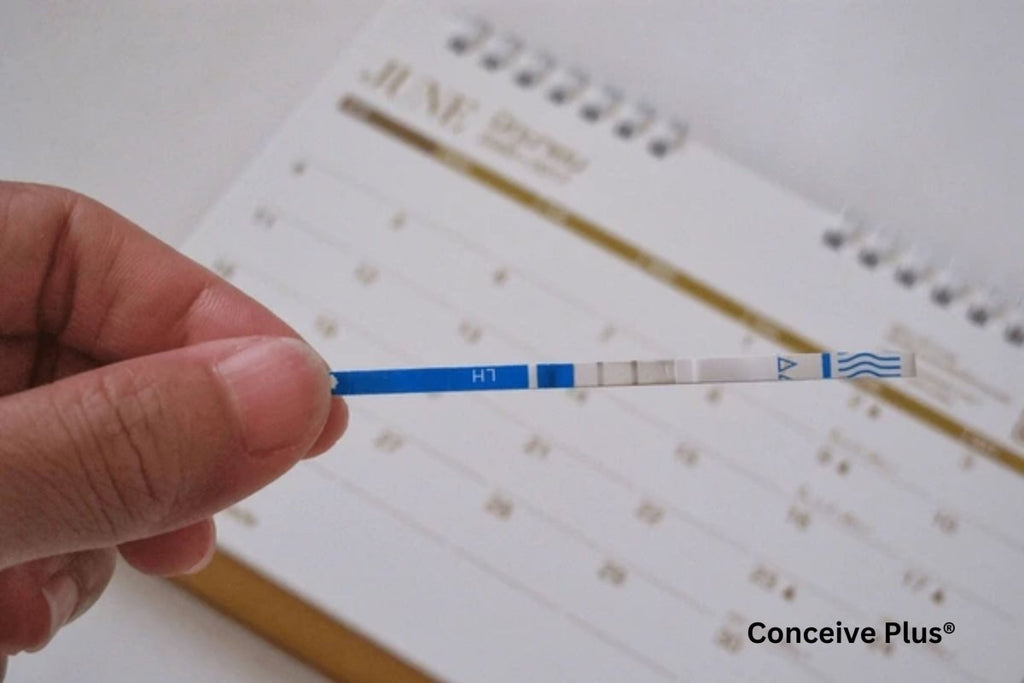
Natural family planning has gained renewed interest in recent years as couples seek to understand their fertility patterns in a non-invasive, holistic manner. Among the various strategies in fertility awareness, one approach stands out for its blend of biological markers and practical observation. Commonly known as the symptothermal method, it offers a means to gauge a woman’s fertile window by combining daily temperature checks with cervical fluid and other bodily signs.
As part of a broader family planning approach, the symptothermal method empowers individuals to make informed reproductive choices by understanding their natural fertility signals. Below is an in-depth exploration of how this practice works, what science says about its efficacy, and the key considerations for those contemplating this method.
Origins and Evolution of a Hybrid Approach
Historically, fertility awareness was often associated with the rhythm technique, which relied on calculating average cycle lengths. However, the rhythm approach alone sometimes led to inaccuracies because menstrual cycles can vary significantly due to stress, illness, and other lifestyle factors. Researchers and health practitioners thus began searching for more reliable markers to identify ovulation. Over time, specific indicators like basal body temperature (BBT) and cervical mucus consistency were studied extensively, leading to the formation of a multi-faceted technique that integrates both data points. By combining these signs with regular cycle charting, couples gain a more precise understanding of the few days in each cycle when conception is most likely.
Modern technology and scientific advancements have refined this hybrid system further. Apps and digital tools now allow users to enter daily readings on their smartphones, generating automated fertility forecasts. Despite these new conveniences, the core principle remains the same: observe the body’s physiological signals to discern when ovulation is likely to occur. This emphasis on real-time biological cues sets this approach apart from earlier methods that relied heavily on long-term cycle averages [1].
The Underlying Science of Temperature Shifts
One of the fundamental components of this method is tracking a woman’s basal body temperature. The body usually experiences a slight temperature rise—ranging from 0.2°F to 0.5°F (around 0.1°C to 0.3°C)—shortly after ovulation. This increase is associated with progesterone, a hormone released by the corpus luteum following the release of an egg. By consistently taking a temperature reading every morning upon waking (before any activity), women can detect a pattern of lower temperatures in the first part of the cycle and a higher plateau post-ovulation.
Reliability hinges on consistency and precision. It is crucial to use a thermometer that measures to at least two decimal places (e.g., 97.45°F rather than 97.4°F). Disturbed sleep, travel across time zones, and alcohol consumption can all affect morning temperature readings, so users of this approach must account for these variables when analyzing charts. This attention to detail empowers couples to confirm ovulation dates more accurately than by using historical cycle lengths alone [2].
Cervical Fluid and Its Telltale Role
Equally essential is monitoring cervical fluid, which changes in texture, color, and volume throughout a woman’s menstrual cycle. At the start of the cycle, after menstruation, many experience dryness or minimal secretions. As estrogen levels rise in the lead-up to ovulation, cervical fluid often appears clearer, stretchy, and more abundant. This egg-white-like consistency facilitates sperm survival and movement, coinciding with the window of peak fertility. After ovulation, rising progesterone typically results in thicker, stickier fluid or a noticeable reduction in discharge.
This set of cues is invaluable since cervical fluid sometimes provides earlier indications of approaching fertility than basal body temperature shifts. By synchronizing these findings with morning temperature readings, users create a holistic snapshot of the cycle’s fertile days. This dual confirmation—a distinctive cervical fluid pattern followed by a temperature rise—offers a higher degree of reassurance about ovulation status than checking either sign alone [3].
Charting and Interpretation
Keeping accurate daily records is at the heart of the sympto thermal method. A typical chart includes columns for date, waking time, basal body temperature, cervical fluid observations, and any additional notes (such as disruptions to sleep, stress events, or illness). With consistent practice, patterns emerge. For example, if a woman notices fertile-quality cervical fluid for three days and then a distinct temperature hike on the fourth, she can mark ovulation as having likely occurred just before the temperature rise.
Determining fertile windows is a multi-step process. Charts help identify which days require abstinence or alternative protection if avoiding pregnancy. Conversely, couples trying to conceive may specifically target the days showcasing fertile cervical fluid before the documented temperature surge. In this manner, the sympto thermal method serves a dual purpose: it can guide either pregnancy achievement or pregnancy prevention.
Efficacy Rates and Scientific Backing
When used correctly and consistently, research has demonstrated that fertility awareness-based methods can yield a contraceptive effectiveness comparable to some barrier methods. A systematic review published in Human Reproduction Update noted that advanced forms of fertility tracking, including the combination of temperature and cervical mucus observations, can have a success rate of over 95% with perfect use. Typical use may see a higher failure rate, but education and clear instructions dramatically enhance reliability.
The method’s adaptability also makes it appealing. Some couples opt to learn under the guidance of a certified instructor for the first few months, ensuring they interpret charts accurately. Others prefer to self-educate through reputable books and online courses, relying on technology for data recording. Regardless of the learning avenue, the common thread is that diligence in tracking and charting correlates strongly with favorable outcomes.
For individuals seeking hormone-free alternatives in family planning, exploring a natural plan B can provide additional reassurance in cases where primary fertility tracking methods require a backup strategy.
Beyond Contraception: Broader Health Insights
Though often discussed primarily as a natural family planning tool, the sympto thermal method also provides valuable insights into a woman’s reproductive health. Tracking basal body temperature patterns can reveal anomalies such as short luteal phases or consistently delayed ovulation. Such irregularities may suggest underlying hormonal imbalances or conditions like polycystic ovary syndrome (PCOS). For instance, consistently low temperatures might point to a thyroid issue, prompting further investigation.
Similarly, changes in cervical fluid that deviate from an established pattern might indicate potential infections or stress-related cycle disruptions. Early recognition of these signals can motivate timely consultations with healthcare providers, making the practice of fertility awareness a convenient form of health monitoring in addition to its contraceptive or conception-oriented role [4].
The Bottom Line
Whether utilized to enhance the likelihood of conception or to avoid pregnancy without hormonal interventions, the symptothermal method stands as a remarkable fusion of physiology and self-awareness. Its success hinges on diligently recording basal temperature, observing cervical fluid, and consistently interpreting the data. For those willing to invest in learning and implementing this method, the rewards can include deeper insight into reproductive health, improved communication with a partner, and a heightened sense of personal agency. Ultimately, the symptothermal method demonstrates how knowledge of the body’s rhythms can shape informed reproductive decisions.
References
- Peters A, Mahdy H. Symptothermal Contraception. [Updated 2023 Nov 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564316/
- Frank-Herrmann P, Heil J, Gnoth C, Toledo E, Baur S, Pyper C, Jenetzky E, Strowitzki T, Freundl G. The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple's sexual behaviour during the fertile time: a prospective longitudinal study. Hum Reprod. 2007 May;22(5):1310-9. doi: 10.1093/humrep/dem003. Epub 2007 Feb 20. PMID: 17314078.
- Katz DF. Human cervical mucus: research update. Am J Obstet Gynecol. 1991 Dec;165(6 Pt 2):1984-6. doi: 10.1016/s0002-9378(11)90559-6. PMID: 1755453.
- Gallagher J. More about natural family planning. Aust Fam Physician. 1983 Nov;12(11):786-92. PMID: 6667188.