When to Take Ovulation Test After Period: A Comprehensive Guide to Pinpointing Fertility

Monitoring fertility is increasingly important for those trying to conceive or seeking deeper insights into reproductive health. Yet, confusion often arises about timing and usage of ovulation predictor kits (OPKs), especially when to take ovulation test after period. This guide clarifies how these tests work, why scheduling matters, and how to interpret results effectively. Whether you are new to family planning or looking to refine your approach, these insights will help you optimize the testing experience.
The Role of Ovulation in Conception
Ovulation is when an ovary releases a mature egg, which survives about 12 to 24 hours. Conception is likeliest if sperm reside in the reproductive tract beforehand, since they can live there for days. Though many assume a “day 14” rule in a 28-day cycle, real variations are common. Factors like stress and hormonal imbalances can shift ovulation earlier or later. Recognizing these shifts helps you stay flexible rather than clinging to a fixed date.
Pinpointing ovulation boosts your likelihood of conceiving and clarifies overall reproductive health. If you notice symptoms like mild pelvic aches or changes in cervical mucus, they can reinforce your OPK findings. Combining physical observations with testing offers a well-rounded perspective on fertility [1].
Understanding How OPKs Function
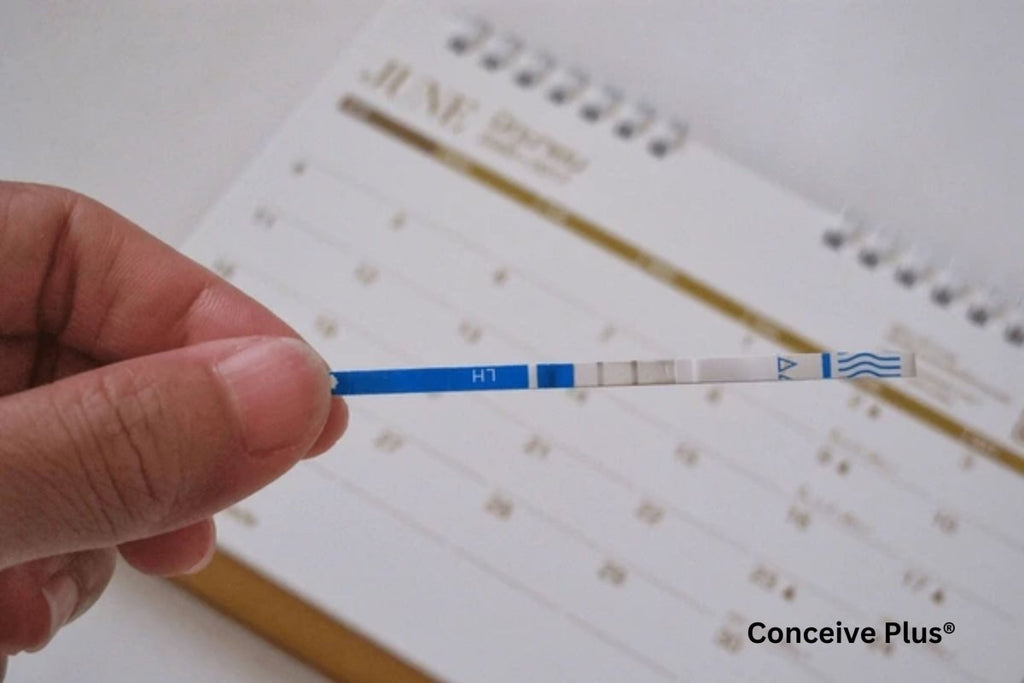
OPKs detect an LH surge that typically precedes ovulation by one to two days. This hormone signals the follicle to release its egg. Different OPKs, from simple strips to digital readers, follow the same principle—when LH levels rise enough, the test registers a positive result. Always check your kit’s specific guidelines, including how to collect urine and interpret lines or symbols. A control line shows the test is valid, while a clear indicator tells you the surge is present [2].
Determining Your Testing Schedule
Most people begin OPK use shortly before the day they expect ovulation. If your cycle is about 28 days and ovulation near day 14, starting around day 10 is typical. For shorter or longer cycles, adjust accordingly. If you have irregular cycles, gather data for a few months or employ secondary indicators like basal body temperature (BBT) to narrow down your likely window.
Your cycle can shift if you alter exercise routines, experience emotional upheavals, or undergo sudden weight changes. To avoid missing a brief LH surge, test daily until you see a clear positive or confirm you’ve passed your fertile window. When the surge appears, ovulation is likely imminent [3].
Tips for Improved Accuracy
Questions often arise about what time of day to take ovulation test samples. Some brands suggest testing later in the day, assuming LH accumulates by midday. Others favor morning due to concentrated urine. Regardless, choose a time you can maintain consistently. The best time of day for ovulation test reliability depends largely on product instructions and personal routine.
Avoid overhydrating just before testing, as excessive fluids may dilute hormones. Follow proper storage recommendations and expiration dates. Keep used strips out of direct light and handle them carefully. Developing a steady process, from fluid intake to test handling, increases the likelihood of detecting your surge without confusion.
Managing Irregular Cycles
Irregular cycles can present considerable challenges for those attempting to pinpoint ovulation. In some cases, hormonal conditions such as polycystic ovary syndrome (PCOS) or thyroid dysfunction lead to unpredictable LH surges, causing test results to vary widely from month to month. Stress, rapid weight changes, and intense exercise routines can also play a role by disrupting hormone production. If you find it difficult to rely on a narrow window for testing, it may help to begin using ovulation tests earlier in your cycle and continue until you either see a surge or your period begins. Although this approach can use more test strips, it is often the most reliable method when ovulation timing is unclear.
For extra assurance that ovulation has taken place, many people track their basal body temperature (BBT). Immediately after ovulation, the release of progesterone typically causes a slight but noticeable rise in morning temperature. If you see this temperature shift following a positive OPK, it indicates that the egg was likely released. On the other hand, if several consecutive cycles pass without an evident LH surge—despite consistent testing—or if you notice significant irregularities in your results, it is wise to consult a healthcare provider. Medical professionals can evaluate potential hormonal imbalances, stress-related factors, or conditions such as endometriosis or PCOS that disrupt your menstrual cycle. Treating these root causes may restore greater predictability, making your ovulation tests more conclusive. By combining thorough medical guidance with flexible testing strategies, you can still gain clarity on your most fertile days despite the inherent challenges of irregular cycles [4].
For individuals with irregular cycles, recognizing signs of ovulation without a period can be crucial in tracking fertility and understanding hormonal fluctuations.
Dealing with Emotional Stress
Trying to conceive is often stressful, and high stress can delay or disrupt ovulation. If you keep missing the LH surge, or if negative results repeat, frustration can build. A well-structured plan regarding when to start taking ovulation tests may lessen anxiety. Record each outcome, note any physical signs, and consider testing twice daily near the presumed fertile window if you suspect a short surge.
If uncertainty lingers, seeking professional advice can ease worries. Doctors can perform tests to confirm if ovulation is occurring. Even if your schedule or lifestyle is hectic, establishing a consistent OPK routine helps you adapt to monthly fluctuations more calmly.
Advanced Tools and Combined Methods
Beyond OPKs, a range of apps and wearables log fertility clues like heart rate and skin temperature. These tools may offer reminders or analytics to predict your fertile window. Yet no technology is infallible. If an app’s forecast contradicts your actual test results, trust the evidence that physical tracking provides. Over time, updates to your app based on verified data can align digital predictions with real patterns.
For those who appreciate deeper detail, combining OPKs with methods such as BBT tracking or cervical mucus observation paints a fuller picture. If these signs consistently match your LH surge, it reinforces confidence in your timeline. Conversely, irregularities might indicate a need for medical follow-up [5].
Understanding the connection between ovulation and pregnancy test accuracy can further clarify how hormonal changes influence test results and fertility tracking.
Additional Practical Tips
Users frequently ask about the best time of day to take ovulation test readings in a busy life. Some find midday feasible, while others prefer the morning before routine tasks pile up. Whichever slot you choose, consistency is key—testing at random times makes it harder to compare results from one day to the next. Jotting down times and outcomes, or using digital trackers, simplifies pattern recognition.
Lifestyle elements, such as diet and moderate exercise, also influence fertility. Extreme regimens can alter hormone levels and shift ovulation. Certain medications—especially fertility drugs—may affect LH readings. If in doubt, consult a professional about their potential impact on test accuracy. Detailed notes about your cycle, habits, and test results help pinpoint any recurring challenges.
Supplementary Health Checks and Professional Guidance
Beyond routine ovulation testing, regular health evaluations can uncover critical factors that might influence fertility. For instance, blood tests can detect thyroid malfunctions or elevated prolactin levels, both of which can disrupt menstrual cycles. A physician may also order ultrasounds to assess the ovaries and uterus, ensuring no structural issues impede conception. In some cases, subtle symptoms such as irregular bleeding or significant pelvic pain hint at conditions like fibroids or endometriosis, which can complicate ovulation tracking.
It is also worth discussing your overall lifestyle with a healthcare provider. Excessive caffeine, smoking, or certain prescription medications can hamper reproductive health. Meanwhile, nutrient deficiencies—particularly in iron or vitamin D—may alter hormonal balance. By addressing these areas, you set a supportive foundation for more accurate OPK results. If you have a partner, encouraging them to undergo basic evaluations can be equally important, since sperm quality influences your chances of successful fertilization.
A medical professional can help interpret confusing data if you find repeated negative tests, unpredictable surges, or sporadic cycles despite seemingly correct OPK usage. They may suggest a monitored cycle, in which tests and ultrasounds pinpoint when ovulation occurs. This provides a definitive reference point to compare with your at-home findings. Additionally, a fertility specialist can recommend personalized interventions and discuss assisted reproductive options if underlying issues persist. In short, pairing proactive health checks with diligent ovulation testing ensures you tackle potential obstacles early, making the road to conception or cycle understanding as clear as possible [6].
The Bottom Line
A common question is when to take ovulation test after period. Usually, this aligns with cycle length. If you suspect ovulation on day 14, starting on day 10 creates a comfortable window for detecting the surge. Those with shorter cycles begin earlier, and longer cycles might wait an extra day or two. Some keep testing daily until a definite LH surge appears. If none emerges, continuing until menstruation rules out a late peak.
When you confidently know when to take ovulation test after period, you possess greater control over your reproductive path. Observing how factors like stress or fitness routines affect each cycle equips you to make informed choices. If consistent testing fails to reveal a surge, a professional evaluation can uncover hidden issues.
Ultimately, OPKs serve as practical tools to help you identify peak fertility. Combine them with consistent habits, awareness of bodily cues, and a willingness to adapt to monthly fluctuations. If digital aids appeal to you, let them complement rather than override your actual test findings. By tracking each cycle’s nuances, you steadily increase your odds of catching the LH surge at precisely the right time. In doing so, you build confidence in your journey toward conception or a clearer understanding of your cycle—one that emerges through patience, accurate testing, and mindful observation.
References
- Su HW, Yi YC, Wei TY, Chang TC, Cheng CM. Detection of ovulation, a review of currently available methods. Bioeng Transl Med. 2017 May 16;2(3):238-246. doi: 10.1002/btm2.10058. PMID: 29313033; PMCID: PMC5689497.
- Yeh PT, Kennedy CE, Van der Poel S, Matsaseng T, Bernard L, Narasimhan M. Should home-based ovulation predictor kits be offered as an additional approach for fertility management for women and couples desiring pregnancy? A systematic review and meta-analysis. BMJ Glob Health. 2019 Apr 25;4(2):e001403. doi: 10.1136/bmjgh-2019-001403. PMID: 31139458; PMCID: PMC6509595.
- Su HW, Yi YC, Wei TY, Chang TC, Cheng CM. Detection of ovulation, a review of currently available methods. Bioeng Transl Med. 2017 May 16;2(3):238-246. doi: 10.1002/btm2.10058. PMID: 29313033; PMCID: PMC5689497.
- Kolstad HA, Bonde JP, Hjøllund NH, Jensen TK, Henriksen TB, Ernst E, Giwercman A, Skakkebaek NE, Olsen J. Menstrual cycle pattern and fertility: a prospective follow-up study of pregnancy and early embryonal loss in 295 couples who were planning their first pregnancy. Fertil Steril. 1999 Mar;71(3):490-6. doi: 10.1016/s0015-0282(98)00474-9. PMID: 10065787.
- Nobles J, Cannon L, Wilcox AJ. Menstrual irregularity as a biological limit to early pregnancy awareness. Proc Natl Acad Sci U S A. 2022 Jan 4;119(1):e2113762118. doi: 10.1073/pnas.2113762118. PMID: 34969843; PMCID: PMC8740731.
- Ebinghaus M, Agricola CJ, Schmittinger J, Makarova N, Zyriax BC. Assessment of women's needs, wishes and preferences regarding interprofessional guidance on nutrition in pregnancy - a qualitative study. BMC Pregnancy Childbirth. 2024 Feb 21;24(1):154. doi: 10.1186/s12884-024-06351-z. PMID: 38383376; PMCID: PMC10880225.